DOWNLOAD FULL JOURNAL
Volume 00, Number 00, 2021 ª Mary Ann Liebert, Inc.
DOI: 10.1089/jayao.2021.0036
1 Joseph Kirk, BScKin, Jodie Jespersen, RN, 2 and Sarah McKillop, MD, MSc3,i
This retrospective chart review assesses the impact of introduction of an adolescent young adult oncology navigator (AYAON) on first contact with oncology psychosocial services (OPS) for adolescents and young adults (AYAs) newly diagnosed with cancer. All AYAs newly diagnosed at a single adult oncology center between 17 and 29 years of age from July 2016 to July 2018 were reviewed. AYA contact with the AYAON was associated with an increase in contact with OPS. Following the introduction of the AYAON, there was a clinically significant decrease in the time to first OPS contact for newly diagnosed AYAs with cancer.
Keywords: navigator, young adults with cancer, psychosocial, early contact.
Introduction
Adolescents and young adults (AYAs) are a recognized and distinct population, typically 15–39 years of age, with their own unique care needs. These unique needs are further complicated through the lens of cancer. Among AYAs, cancer is the leading cause of nonaccidental death; thus, care for AYAs with cancer (AYAC) is a relevant concern warranting a tailored approach. 1–3 The Canadian Task Force on AYAC concluded AYAC were likely to benefit from psychosocial care due to an increased incidence of distress, anxiety, and depression reported in this population.4
AYAC have been identified as having an increased risk of psychiatric conditions, including anxiety, depression, substance abuse, and suicide. 2 Almost half of AYAC survivors report an unmet need for psychosocial support 2 and many perceive a need for additional psychological support. 1 The increased psychosocial distress among AYAC compared to AYAs without cancer is alarming and a threat to the ‘‘pursuit of normal,’’ which is thought to be uniquely important to the AYA group as a whole.5
One approach to improving access to oncology psychosocial services (OPS) by AYAC is the introduction of an AYA Navigator within the cancer center. A patient navigator can help with translating health information, communicating with the patient’s health care team, and helping to facilitate access to support services. 1 The patient navigator role was
designed to assist a patient population in overcoming barriers to health care, reducing distress, and enhancing the quality of life for the patient and their family.1
Patient navigation is an effective strategy to improve many aspects of oncology care, including support, patient satisfaction, and the utilization of available health resources.6 Based on a review of the literature, there is no evidence evaluating the effectiveness of patient navigators in improving the AYAC care or improving access by AYAC to OPS. 6 It is recommended that oncology centers provide
AYAC with patient navigators to facilitate their experience within the health care system.7
An AYA oncology navigator (AYAON) was introduced at the Cross Cancer Institute (CCI) in Edmonton, Alberta, in May 2017. The goal of the AYAON is to connect with all AYAs newly diagnosed with cancer as soon as possible after referral to the cancer center. It was hoped that the AYAON would facilitate early access to support services for AYAC.
The purpose of this study was to identify changes in early first contact with OPS following the introduction of the AYAON at the CCI. It was hypothesized that the introduction of the AYAON role would both increase the incidence of OPS contact and decrease the time to the first contact with the OPS for AYAs newly diagnosed with cancer. The primary objective was to determine the incidence of contact with the OPS by AYAC (17–29 years) diagnosed and treated at the CCI between July 2016 and 2018. The secondary objectives were to assess if the introduction of the AYAON role had an impact on (1) the incidence of contact with OPS and (2) the time from diagnosis and first oncology consult to first contact with the OPS by AYAC.
2 KIRK ET AL.
Table 1. Patient Demographics (n = 195)
AYAON, adolescent young adult oncology navigator.
Methods
Following study approval by the Health Research Ethics Board of Alberta—Cancer Committee, the Alberta Cancer Registry provided a list of all patients diagnosed and treated at the CCI between July 2016 and 2018, 17 to 29 years of age, at the time of an initial cancer diagnosis. This list was combined with the AYAON’s list of patients contacted to ensure a complete patient list for review. Patients were excluded if they were never seen for consultation or treatment at the CCI, or if they were deceased <1 month from the diagnosis of cancer.
A retrospective chart review using the electronic medical records was completed. Data collected included patient demographics, AYAON contact, first OPS contact (including social work, psychology, and spiritual care), and the primary cancer diagnosis. Statistical analysis was performed using a general database management system, SPSS statistical software, and descriptive statistics.
Results
A total of 195 AYAs newly diagnosed with cancer were available for review (Table 1). Of these, 87 were male and 109 were female with a median age of 25 years (range 17–29
EARLY PSYCHOSOCIAL CONTACT: AYA NAVIGATOR IMPACT
years). Two thirds of the included AYAC were between 24 and 29 years of age. Three quarters of the AYAC reviewed had contact with the AYAON. A third of AYAC were diagnosed before the AYAON navigator was introduced in May of 2017, but 40% were subsequently contacted by the AYAON. Ninety percent of AYAs diagnosed after May 2017 had AYAON contact. Hematologic malignancies accounted for 32% of the included AYAC followed by endocrine malignancies (18%), genitourinary malignancies (16%), breast cancers (7.7%), gynecological malignancies (7.7%), central nervous system tumors (6%), followed by sarcomas, melanoma, head and neck, and lung cancer (Table 1).
Of the 48% of AYAC who met with OPS, 83% met with social work, 17% met with psychology, and <1% met with pastoral care. Significantly more AYAC in the younger age group (17–23 years) connected with OPS (64%) compared to 46% of the older (24–29 years) AYAC ( p = 0.035).
content goes here. Edit or remove this text inline or in the module Content settings. You can also style every aspect of this content in the module Design settings and even apply custom CSS to this text in the module Advanced settings.
There was a statistically significant difference in OPS contact based on tumor group (Fig. 1). There was OPS contact of all AYAC diagnosed with a lung cancer, for 87% of those diagnosed with a sarcoma, for 3/4 of those with a breast or central nervous system tumor, and for 2/3 of those with a head and neck or hematologic malignancy, <50% of AYAC diagnosed with a genitourinary cancer (42%) and 1/3 of those with a gynecologic cancer (1/3) had OPS contact. Unfortunately, <20% of AYAC with an endocrine tumor and none diagnosed with a cutaneous malignancy had OPS contact ( p < 0.001).
Of the AYAC who met the AYAON, 61% had OPS contact compared with only 27% of the AYAC with no AYAON
contact ( p < 0.001). The median time from diagnosis to initial OPS contact was 44 days. The median time from first consult at the CCI to initial OPS contact was 14 days. The decrease in median time from both diagnosis ( p = 0.056) and oncology consult ( p = 0.058) to the initial OPS contact, following the introduction of the AYAON role, shows a clinically significant trend (Fig. 2). Meeting with the AYAON did not change the median time to first OPS contact for AYAC. There was no significant difference in time to first OPS contact based on being in the younger or older age grouping.
Discussion
Cancer and cancer treatments have the potential to affect the developing psychosocial successes of AYAC by altering their dreams and ambitions. 8 Appropriate access to psychosocial resources potentially improves the long-term psychosocial outcomes of AYAC. The Canadian Task Force on AYAC highlighted the ‘‘unique psychosocial needs that must be met to enable each [AYAC] to reach their full potential,’’ and recommends access to expert psychosocial care for all AYAC. Approximately half of newly diagnosed AYAC in our study received psychosocial care between 2016 and 2018. This is higher than the local older adult (over 29 years old) oncology population with less than a third having OPS contact, but all having access to OPS and lower than the local pediatric oncology population where 100% have OPS contact early after diagnosis.
While the role of the AYAON has not been validated in the literature, in scoping reviews, the provision of emotional,
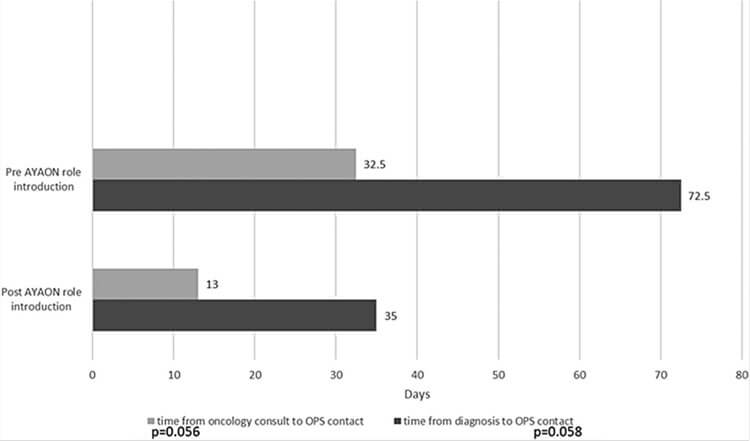
FIG. 2. Clinically significant trend—presence of the AYAON decreased median time to OPS contact. time from diagnosis to OPS contact. time from oncology consult to OPS contact. X axis, AYAON role introduction; Y axis, days; time from diagnosis to OPS contact p = 0.058, time from oncology consult to OPS contact p = 0.056. AYAON, adolescent young adult oncology navigator.
4 KIRK ET AL.
social, and peer support as well as coordinating services ‘‘to fill in the gaps in AYA care’’ are seen as highly valuable aspects of a AYAON role by AYAC and care providers.9,10 In a randomized control trial of adults newly diagnosed with cancer, those with additional patient navigation support were found to have lower use of supportive cancer care, but reported improved patient experience and measured self efficacy.12
In our study, the introduction of an AYAON in the adult cancer center increased the incidence of contact with the OPS for AYAC. The AYAC who connected with an AYAON were twice as likely to have contact with OPS. This suggests that contact with the AYAON is important to facilitate the AYAC connection with OPS, perhaps through increased awareness and assisted access. Further longitudinal study is needed to determine if increased early contact with OPS by AYAC improves both the short- and long-term psychosocial outcomes for this population and their patient experience.
There was an improvement in the median time from initial diagnosis and initial oncology consult to the first OPS contact for AYAs based solely on the introduction of the AYAON program within the adult cancer center. Clinically, there was a shorter time to OPS contact for AYAC who also had AYAON contact (14 vs. 31 days without AYAON contact) as often referrals were directly communicated to the OPS service, however, this did not show statistical significance.
The decrease in time to OPS contact for AYAC following the introduction of the AYAON is likely attributable to the education and awareness-raising activities directed to staff members of the adult cancer center during the AYAON launch process, focusing on the importance of early OPS support for all AYAC. It is reassuring that referral to OPS by the AYAON is not essential to the improved OPS contact for this population. The limitations of standard wait times within the OPS services represent a confounder in this analysis.
When comparing the incidence of contact by AYAC with the OPS by age group, the younger group, 17–23 years old, had significantly more OPS contact compared to the older group (24–29 years old). The reason for this difference is not clear. We hypothesize that the younger group may have had more parental support and advocacy to seek out OPS. In addition, there is often the need for assistance with issues around school absence or insurance coverage transitions that require OPS assistance. The variation in OPS contact by age group is an area that requires investigations to both optimize OPS utilization and to better evaluate the needs of the AYAC cohorts for OPS by age group.
We found a significant variation in OPS contact based on tumor diagnosis. The Canadian Task Force on AYAC advocates for every AYAC to have psychosocial support and recognizes that the prescribed cancer therapies cannot be directly correlated with predicted psychosocial needs. 4 There are likely multiple confounders to this finding, including the types of treatment prescribed; however, based on the small sample size, further analysis of this variation is not possible. The difference in OPS contact by tumor group is important to consider and will be a focus for further study and an institutional quality improvement project.
This is a single-center retrospective chart review for which we used descriptive statistics due to the relatively small sample size available for analysis. This is a limitation of this study. While there is the ability to compare the incidence of
OPS contact and time to contact for AYAC before and following the introduction of the AYAON, the contact with AYAON by AYAC in the study was not controlled for. Many AYAC diagnosed before the start of the AYAON still met with the AYAON and there were AYAs who chose to never meet with the AYAON. This introduces additional confounders to the results.
The age range for this study was based on the provincially accepted AYAC definition for the time period of the study based on human resources. This reported AYAC group does, however, reflect the most common cancer types in this age range. 12 This study unfortunately excludes data for the older
AYAC age group (30–39 years). As the definition of AYAC has now changed in the province to include those 15–39 years of age, we will reevaluate OPS contact for the entire population. The retrospective findings presented in this study are important in informing the development of future research on the impact of the AYAON and early OPS contact on the psychosocial well-being of AYAC, the AYAC cancer experience, and the adult oncology center resource utilization.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
No funding was received for this article.
References
1. LaRosa K, Stern M, Bleck J, et al. Adolescent and young adult patients with cancer: perceptions of care. J Adolesc Young Adult Oncol. 2017;6(4):512–8.
2. Institute of Medicine. Identifying and addressing the needs of adolescents and young adults with cancer: workshop summary. Washington: The National Academies Press; 2013.
3. Coccia PF, Pappo AS, Beaupin L, et al. Adolescent and young adult oncology, version 2.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2018;16(1):66–97.
4. Fernandez C, Fraser G, Freeman C, et al. Principles and recommendations for the provision of healthcare in Canada to adolescent and young adult-aged cancer patients and survivors. J Adolesc Young Adult Oncol. 2011;1(1): 53–9.
5. Smith S, Mooney S, Cable M, Taylor R (Eds). The blueprint of care for teenagers and young adults with cancer, 2nd ed. London: Teen Cancer Trust; 2016.
6. Shejila C, Mamatha S, Fernandes D. Oncology nurse navigator programme—a narrative review. J Health Allied Sci NU. 2015;5(1):103–7.
7. Ramphal R, Aubin S, Czaykowski P, et al. Adolescent and young cancer: principles of care. Curr Oncol. 2016;23(3): 204–9.
8. Docherty S, Kayle M, Maslow G, Santacroce S. The adolescent and young adult with cancer: a developmental life course perspective. Semin Oncol Nurs. 2015;31(3): 186–96.
9. La Rosa K, Stern M, Lynn C, et al. Provider perceptions’ of a patient navigator for adolescents and young adults with cancer. Support Care Cancer. 2019;27(11):4091–8.
EARLY PSYCHOSOCIAL CONTACT: AYA NAVIGATOR IMPACT
10. Pannier S, Warner E, Fowler B, et al. Age-specific patient navigation preferences among adolescents and young adults with cancer. J Cancer Educ. 2019;34(2):242–51.
11. Berezowska A, Passchier E, Bleiker E. Professional patient navigation in a hospital setting: a randomized controlled trial. Support Care Cancer. 2021;29(4):2111–23.
12. Horner M, Ries L, Krapcho M, et al. SEER cancer statistics review, 1975–2006. Bethesda, MD: National Cancer Institute; 2008. Accessed May 24, 2018 from: www.joplink .net/prev/201003/ref/16-001.html
Address correspondence to: Sarah McKillop, MD, MSc Cross Cancer Institute University of Alberta Department of Pediatrics 11560 University Avenue NW Edmonton T6G1Z2 Alberta Canada
Email: sarah.mckillop@ahs.ca
A Guide For Young People Facing Cancer
So, you have cancer. Now What…?
Whether you have just been diagnosed, are already receiving treatment, or have completed most of your treatment, there are probably so many things running through your head all at the same time — questions, feelings, new thoughts —
As hard as it might be to focus on anything, there are a few things that might help you get a better handle on the situation.
This book is designed to help you get a handle on some of what is going on and give you some tips for dealing with the massive challenges your cancer diagnosis has thrown at you.
Give Today
Contact Us
Fax: 817-698-8471


Recent Comments